Stewart said his depression likely started in high school, stemming from bullying and his stepfather’s suicide, but went undiagnosed until he came to Chapel Hill. The safety plan he drew up at CAPS is what prompted Stewart to check himself into the hospital when, after a day of binging on food and alcohol, he attempted to hang himself with a belt in his bedroom.
While Stewart’s experience with CAPS was positive, some, like sophomore Christian Lutz, 20, think the University isn’t doing enough to help those dealing with mental illness.
Lutz, a public policy and environmental science double-major from Lawndale, has been a financially independent student for nearly a year following a fallout with his parents. He said he felt depression creeping into his life around that time, but struggled to treat his illness despite counseling from CAPS.
At first, Lutz wasn’t sure if he was depressed or simply sad, lonely or stressed. His depression often feels like being enclosed in a pitch black box, unable to see forward or backward, only able to exist in a moment of darkness. That social isolation can make it seemingly impossible to socialize, complete assignments, eat or leave home for days at a time.
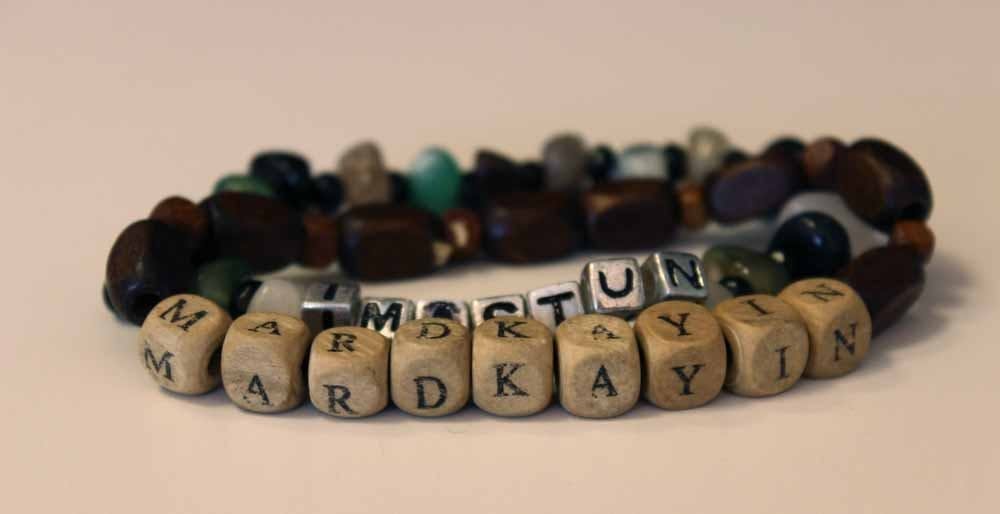
“I think part of combating mental illness is making sure people know that what they do matters,” Lutz said. “A lot of times I thought that things I did didn’t matter, or if I wasn’t here it wouldn’t make a difference. But of course, everybody has touched someone’s life before. Everybody is interconnected.”
Likely due to the general stigma around mental health, though, Lutz thinks many UNC-CH students are unaware of what CAPS does or how to access its services. And for those who do go to CAPS, it isn’t always a sure fit.
“A lot of what CAPS does is good, but I think they could do more and better with how they handle students and their mental health,” Lutz said.
While CAPS appointments have swelled in recent years, students like Lutz argue that due to budget cuts, many students aren’t afforded the personal care they require to treat their illnesses. Beyond that, treating mental illnesses isn’t always as clear cut as treating physical ones with pain medications. Anti-anxiety and depression medications aren’t one-size-fits-all, and often come with a slew of side effects.
Former UNC-CH student Timothy Wyatt, 22, said he started to struggle with his mental health as a first-year living in Koury Residence Hall. He saw himself as the caretaker type, even going so far as to help a hallmate through a cocaine overdose and talking another classmate off the top of a parking deck following a conflict with an abusive boyfriend.
The Burnsville native enrolled in college in relatively good mental health. After a semester of helping friends with their mental health, though, he felt his mental wellness declining. Soon, he was going to CAPS to ward off depressive thoughts and struggling to put food in his mouth or get out of bed in the morning.
As a first-year, Wyatt’s depression worsened until he threatened to take his own life. His roommate called the police from their dorm. Wyatt ran. They caught him a mile later, and he was placed under mandatory psychiatric care.
He said while his experience at CAPS could’ve been better, the impetus for change must come from the university as a whole – from the school’s administration to the student body.
To get the day's news and headlines in your inbox each morning, sign up for our email newsletters.
“Students have to have each other’s backs,” he said. “People don’t realize the importance of reaching out, of having groups of people you can go to and say, ‘Come on, let’s go get food, let’s hang out, let’s deal with and talk about these things.’”
Kelsie Qua, 25, said she doesn't fault the University or think it’s the school’s responsibility to manage students’ mental and physical health. She does, however, have a problem with the way mental health services are being presented.
Qua suffers from anxiety and depression. She got caught in the Catch-22 of prescription drugs: one side effect of her medication was an uptick in suicidal thoughts. She eventually checked herself into the hospital for treatment at 21.
With the help of counselors, Qua learned coping skills to deal with her anxiety and depression, attended community college and later was accepted to UNC-CH.
In the summer before her arrival in Chapel Hill, Qua called the office of Accessibility Resources & Service about managing anxiety on campus. When she called at first, she received no response.
After waiting through dial tones and attempting to leave a message, she finally got through – only to be told the office was understaffed and that she should call back later.
“When you have a condition like anxiety that’s totally invisible, it’s already hard for people to take you seriously,” Qua said. “It’s hard to say, ‘This is something that affects me every single day, and I need help with it.’ And hearing someone say, ‘I have 20,000 other students to deal with’ left a really bad taste in my mouth. I immediately got the sense that my issues didn’t matter.”
Tiffany Bailey, director of Accessibility Resources & Service, said between 1,300 and 1,400 undergraduate and graduate students receive accommodation from ARS. She said her office doesn’t track the exact breakdown of between students with physical disabilities and those with mental ones, but Bailey said that over the last five years, there’s been an uptick in students applying for aid with psychological and chronic medical conditions.
Especially for students suffering from mental illness, Bailey said ARS looks at students on an individual basis to determine their specific symptoms, limitations and needs. Accommodations often include flexibility on attendance, exam-taking or assignment deadlines.
In response to Qua’s story from last summer, Bailey said her department has never intended to make a student feel like less than a priority. However, she also said ARS is a department that gets especially hectic during the summer, and last year, operated with just four full-time employees.
Bailey said the story doesn’t surprise her, but that she hopes students give ARS some leeway.
“We don’t want people to feel bad, but we don’t want to just let the phone ring,” Bailey said. “We always want to acknowledge, ‘Yes, we’re here, but this is the situation, can you give us a call back?’ Obviously, our intent was not to be negatively impacting the student.”
CAPS itself has been under pressure lately, too. Facing budget cuts from the University, CAPS psychiatrist and director Allen O’Barr said his office is focusing on affording suicidal students same-day care.
In an interview with The Daily Tar Heel from January, O’Barr said suicides can’t necessarily be prevented. While his department’s preventive efforts doubtlessly help those battling anxiety disorders, there’s not always a clear, long-term solution to the daily battle.
“Unfortunately we’re dealing with this every day, multiple times a day,” he said. “Despite that, periodically a suicide occurs, and we try to look at that as closely as we can to try to determine, ‘Is there anything here that could have been different?’”
The ideal response to depression is unclear, but when those suffering from mental illness describe their trauma, however, that pain is undeniably vivid.
Stewart said his depression is an internal battle between holding on to hope and humanity versus giving in to pain.
“It’s like being caught in a river. It’s flowing so fast and so strong, and you know that you’ll be swept away,” he said. “But there’s a rock right in the middle of the river, and you’re trying your hardest to hang onto it, but it’s so hard. Your arms and body want nothing more to just let go, but you know that you can’t, or it will be your doom.”